Location
Our Washington Location
Our inpatient facility is located in Washington, and will serve Washington state. It will provide a safe & therapeutic environment for both our staff and patients.
- Edmonds
7416 212th St SW,
Edmonds, WA 98026
Disclaimer: This article is not intended as a substitute for the counsel of a qualified physician or licensed therapist. This content should be used for purely informational purposes. Please consult your doctor if you have further inquiries on this subject. We intend to impart the most accurate and recent information but cannot make any guarantees.
From the promising career of young Cory Monteith to world-famous superstars like Marilyn Monroe and Judy Garland, entirely too many celebrities have been lost to polysubstance addiction, specifically the mixing of drugs and alcohol.
Although Marilyn's death was ruled a suicide, would she have made that fatal decision if she hadn't already been intoxicated on booze and pills at the time? Polydrug addiction is the deadliest type of substance abuse and steals young lives every single day.
According to the Drug Abuse Warning Network, a fourth of all emergency room visits can be attributed to multi-substance abuse. Up to 70% of all overdoses could be caused by mixing different types of substances, and sometimes it happens completely by accident. An example of this could be an aging individual who decides to have a few drinks while taking strong heart medication.

As of 2013, drug and alcohol overdose became the leading cause of accidental death in the United States. Not all of these overdoses included illicit drugs; some were due to the unintentional combination of alcohol with prescription or over-the-counter medications. Especially for those who have to take medications daily for chronic conditions, drinking any alcohol at all can be a risk. Do you know which medications are safe to take with alcohol? If not, a future mistake could be devastating.
This article will describe the risks of polydrug use that involve mixing alcohol and other substances - both illicit drugs and legal medications.
Alcohol, all by itself, does a number on your brain and body. First, it crosses the blood-brain barrier within minutes of taking the first drink and begins releasing the "happy chemical" dopamine into your brain. This neurotransmitter is what causes the euphoric feeling associated with drinking. At the same time, your stomach will be working hard to neutralize the caustic chemicals in the ethanol you're drinking, while your liver works frantically to leach the toxins from your bloodstream and dispose of them. All of this happens from the very first drink.
Now, if you add other chemicals, toxins, or medications into the mix, your brain and organ systems will have that much more work to do to keep your body functioning at a healthy balance. Sometimes, it is simply too much for your body to handle, and something falls through the cracks. That's when you get sick, vomit, pass out, or in the worst cases, overdose. This is what could happen when you mix alcohol with other substances or medications.
Do you see how this becomes a problem? Even mild over-the-counter (OTC) medications like Tylenol can have negative interactions with alcohol. Your body simply wasn't made to process foreign chemicals and intoxicants, especially in multiple combinations. Risk of drug overdose aside, the risk of alcohol poisoning also greatly increases when other substances are taken at the same time, whether it's a street drug or a common medicine.
The short answer to this question is yes, some individuals are at greater risk of complications when combining alcohol with other substances. While the practice is dangerous for anyone, some people have to be even more cautious than others.
People of advanced age are at an especially high risk of unhealthy reactions to a combination of alcohol and drugs. For one thing, as people advance in age, they are more likely to develop chronic conditions like heart disease, osteoporosis, or diabetes. Since the medications for chronic conditions must usually be taken on a daily basis, any amount of alcohol consumed has a chance of interacting with these medications.
Another problem is that, as the body ages, it begins to process and metabolize alcohol more slowly. The older a person is, the harder it is for them to digest alcohol and medications. This means that the substances can build up in the system over time, and any excess or dangerous combination of substances will be more likely to overwhelm the body's systems before they can be metabolized. This results in a much higher risk of overdose or alcohol poisoning than would exist for a younger individual ingesting the same combination of substances.
In most aspects of life, women and men can consider themselves equals, but not when it comes to alcohol. As you may have guessed, women tend to weigh less and have less body mass than men, meaning that they can feel the effects of alcohol faster, but that is not the only factor at play.
Women of all shapes and sizes are simply constructed differently than men. Their bodies have a much higher fat to water ratio, no matter their body type. For this reason, a woman will reach a higher blood alcohol content at a faster rate than a man after drinking the same quantity, even if they are matched pound for pound in weight and size. The same goes for drugs and medications. Equality issues aside, women must take extra care when drinking, especially if they are taking other medications or substances at the same time.

Most people who have experimented with alcohol have a story (or three) about that time they ended up sleeping next to the toilet bowl as a result of drinking three different types of alcohol in one evening. After all, the saying goes, "Beer before liquor, never been sicker."
Does this old adage actually hold true? Well, yes and no. It is true that moving from drinks of a lower alcohol content - like beer or wine - to hard liquor like whisky or rum can definitely lead to over-drinking. This is not really because of the kind of alcohol you are partaking in as much as it is about alcohol content.
You see, if you start the evening by taking a few shots of tequila, you will likely feel the effects very quickly. After that, if you switch to beer, you are slowing down your intake of alcohol, giving your body more time to process the amount you are drinking. Drinking lower-alcohol-content beverages also means that you will have more time to feel the effects of each drink and slow down or stop before getting too intoxicated.
On the other hand, if you start with a glass or two of wine and then move on to shots of hard liquor, you will be greatly increasing your intake of alcohol at a faster rate. Your body will not have time to metabolize the alcohol before it's too late, and you are more likely to end up sick or with a nasty hangover the next morning.
So, it's not really about the kinds of alcohol you mix together, but the overall amount of alcohol you ingest and how quickly.
Some of the drugs responsible for today's opioid epidemic are common medications prescribed by doctors, often after a surgery or injury. Unfortunately, even when prescribed in acceptable and perfectly legal circumstances, opioid painkillers can be incredibly addictive because of the strong effects they have on the neural pathways of the brain. These include drugs like:

Opioids and alcohol are one of the most dangerous polydrug combinations because they both affect the brain in a similar way, causing double the trouble when mixed. Both opioids and alcohol have a depressive effect on the central nervous system (CNS). This is the part of the nervous system that controls breathing, heartbeat, coordination, and most other unconscious processes that keep us alive. When opioids or alcohol are ingested on their own, the brain can usually metabolize them fast enough to neutralize their effects on the CNS and prevent any problems. When taken together however, two substances that depress the CNS system will slow down these processes, creating a hazardous slowing of the body's most important functions. If too much of either drug comes into the body, overdose can occur easily and the CNS system can fail; breathing and or heartbeat will slow to a stop, and it's all over.
If you take opioids for any reason, never ever mix them with so much as one alcoholic beverage. That is one mistake you might not come back from.
Heroin is another opioid, like those named above, but the main difference is that heroin is the illegal form of the drug that is manufactured and sold on the street. Heroin is also a CNS depressant, making it a dangerous substance to mix with alcohol.

One important distinction between heroin and opioid painkillers is that heroin is often cut and diluted with other substances, making it very difficult to ascertain exactly how much heroin is in each dose. This makes it even more volatile and unpredictable when mixed with alcohol. Overdose after combining these two substances is common and often deadly. Here are some other potential side effects of this combination:
Most everyone is familiar with common OTC pain relievers. They are not narcotic or addictive and may be purchased without a prescription. This class of medicine includes household names such as:
As innocuous as these medications may seem, they can still be hard on organs like the kidneys and liver, especially if taken very often. Many people don't realize the strain it puts on the body to mix everyday pain relievers with alcohol, and they pop a few Tylenol after a long night out drinking without a second thought. This is a bad idea. First of all, this combination will cause your blood alcohol levels to jump higher than normal since your body won't be able to to process it as quickly. Other potential side effects include:
Be mindful not to drink for at least four hours after taking a pain reliever, and vice versa.
Anxiety is a commonly diagnosed condition in our society, and the medications that can treat it are numerous. For the purposes of this article, we'll focus on the primary two types of medications prescribed for anxiety - benzodiazepines and beta blockers. For anyone who suffers from chronic social anxiety, panic attacks, or stress-induced hypertension, these types of medications will need to be taken on a daily basis. These are some of the most prevalent anxiety prescriptions:

Most of these solutions work by relaxing certain parts of the brain to counteract the neurotransmitters that cause anxiety; but they also depress the CNS, similarly to the way opioids do. Once again, depressants are exceedingly dangerous to stack on top of one another, which is why alcohol should not be mixed with anxiety meds. Not only could the combination cause overdose; it may also create the following side effects:
Muscle relaxers are commonly prescribed after surgery or to soothe back pain and spinal pressure. They work by relaxing the CNS and taking some of the tension out of joints and muscles. This impact on the CNS makes it risky to mix muscle relaxers with alcohol because of the double-depressant effect mentioned previously. Besides overdose, some of the problems associated with mixing muscle relaxers and alcohol are:
Just like mixing alcohol with opioids, the combination of sleep aids and alcohol is lethal. Most sleep aids are strong CNS depressants that put the brain in a state of deep relaxation. These are some of the most popular brands:

When these two CNS depressants are combined, the brain can quickly forget to do its most important duties, such as pumping the heart or expanding the lungs. So strong is the interaction between alcohol and sleep aids that the combination has been used as a method of suicide. Besides the obvious risks, even mixing small amounts of these two substances could result in:
Although these two substances are sometimes mixed unintentionally, even more dangerous is the trend of mixing codeine cough syrup and alcohol to create the drug "purple drank", also known as "sizzurp" or "lean". Popularized in the late 1980s, the treacherous combination wreaks havoc on the brain and certain organ systems. Of course, drinking purple drank also presents a marked risk of overdose.

Less common though no less dangerous is the combination of OTC cough syrup and alcohol, two substances that are sometimes mixed by accident. In large quantities, this mixture may cause vomiting and diarrhea almost immediately. Overdose is also always a danger when mixing alcohol with any type of cold medication, as well as:
Antidepressants, unlike CNS depressants, affect serotonin levels in the brain. The most commonly prescribed antidepressants include:
Since alcohol affects different neurotransmitters than antidepressants do, taking both at the same time can cause various conflicting and confusing messages to affect the brain. One consequence with this incongruity is that alcohol can make antidepressants ineffective, or worse, it can exacerbate the mental or emotional symptoms that the antidepressants were prescribed for. In most cases where antidepressant do not work properly, doctors cite alcohol as the probable cause.
Another possible consequence is that the chemicals in the antidepressants can prevent the body from metabolizing alcohol as quickly, making your blood alcohol content higher than expected. This could possibly lead to alcohol poisoning. Since antidepressants are usually taken on a daily basis, it is advisable to abstain from alcohol while you are taking them.
Most mood-stabilizing medications consist of either MAOI prescriptions or lithium and can have disastrous interactions with alcohol. Anyone who takes this type of medication, especially if it's on a daily basis, should completely refrain from drinking, due to the possible side effects:
Mixing alcohol with prescription stimulants (also known as study aids) may seem counteractive, but the two substances do interact, and not in a good way. Prescription stimulants usually contain some type of amphetamine, a drug that can increase energy, concentration, focus, and productivity. These include prescriptions like:
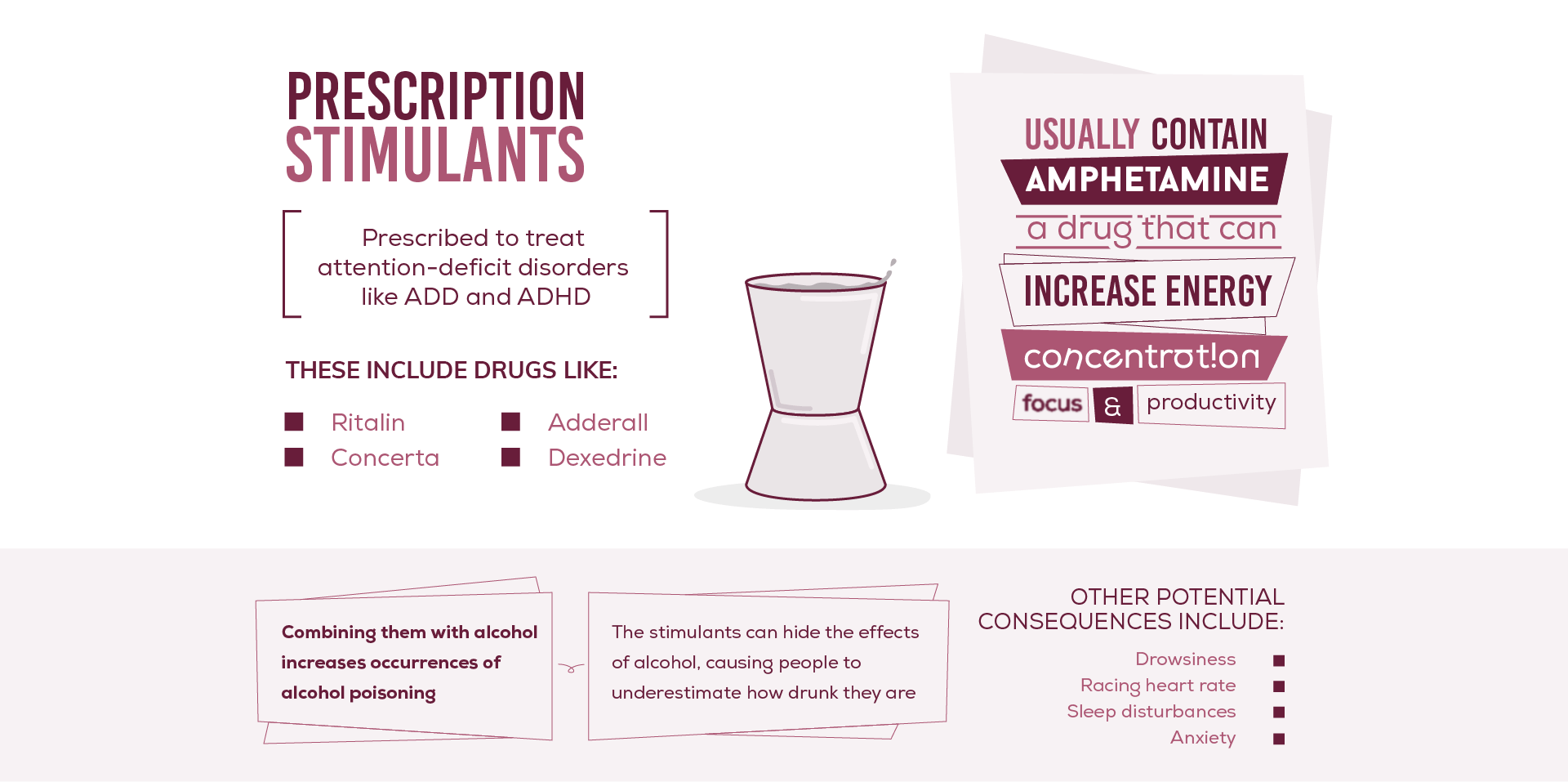
Although they are usually prescribed to treat attention-deficit disorders like ADD and ADHD, some people abuse stimulants in order to increase productivity at work or school. Overly-enthusiastic party goers also use medications like these to stay awake longer for parties, clubs, and raves. This is an especially dangerous practice because it greatly increases the chances that stimulants will be mixed with large quantities of alcohol. This combination increases occurrences of alcohol poisoning since the stimulants can hide the effects of alcohol, masking just how drunk you actually are. Other potential consequences include:
In general, alcohol and diabetes are not good bedfellows. Alcohol is usually packed with sugars and carbohydrates - never a good recipe for anyone with diabetes. For those who take regular medications to control the symptoms of diabetes, alcohol is an even worse idea. Prescriptions like metformin or alpha-glucosidase inhibitors are not compatible with alcohol since they may not work properly when combined with it. When any of these substances are mixed with alcohol, the interaction may cause dangerous dips in blood sugar levels or harmful reactions with lactic acid in the body, either of which may lead to hospitalization.
Anyone with diabetes or prediabetes would be well-advised to consult with a doctor before drinking alcohol at all, especially if they take any of the medications named above.
In some circumstances, it may be safe to have a drink while taking certain arthritis medications, but others, like methotrexate, may cause the following problems:
As with any type of medication, it is absolutely essential that you consult with a doctor before mixing arthritis meds with alcohol.
Like arthritis prescriptions, there are some cholesterol medications that may not have any extreme interactions with alcohol, but every case is different. For example, someone with a history of alcohol abuse or anyone who drinks moderately on a daily basis may face potential side effects if they take cholesterol meds:
Once again, a drink or two while taking cholesterol medications may be okay, but it is important to consult your doctor first.
Whether you're taking medications or not, anyone with heart problems would be well-advised to abstain from drinking alcohol because of the effects it can have on heart rate and general cardiovascular health. Heart medications further complicate the situation because they can have extremely hazardous interactions with alcohol, depending on the the medication. To illustrate, here are some common heart medications and their potential side effects if mixed with alcohol:
There are different types of allergy medications, and they exhibit varying interactions with alcohol. It may be safe to have a drink if you are taking non-drowsy antihistamines like Claritin or Allegra, since they do not affect the CNS. As always, you should never mix any medications with alcohol without talking to your doctor first.
Other sleep-inducing allergy meds like Benadryl, however, should never be mixed with alcohol. Any medication that makes you drowsy very likely depresses the CNS, which means it shouldn't be mixed with alcohol because of the double-depressant effect on the CNS.
No matter what type of allergy meds you're taking, it's best to keep the drinks to a minimum. Even the non-drowsy types may cause nausea and vomiting if mixed with a large quantity of alcohol.
Perhaps the most common type of polydrug abuse, mixing marijuana and alcohol (also known as crossfading) is not as safe as your college roommate would have you believe. While marijuana does not present a high risk of overdose like opioids and illicit stimulants do, it can have very ill effects if mixed with alcohol.

For one thing, both substances are CNS depressants and together, they may slow the heart rate and respiratory processes to dangerous lows. The chances of alcohol poisoning are also higher when combined with weed. Both THC levels and blood alcohol levels are higher than normal when the two are mixed. Another factor is the vomit-inhibiting effect of marijuana, which may prevent the body from vomiting after over-drinking. If the body is unable to vomit excess toxins brought on by over-drinking, the chances of alcohol poisoning are higher still.
Some other possible side effects are:
Illicit drugs present many health risks even when taken alone. Any time you mix street drugs with other substances, you're putting your life in even more danger. Cocaine and other illicit stimulants are no exception.

The most popular illicit stimulants are cocaine and ecstasy, also known as MDMA. These are widespread party drugs that have become part of the club and rave culture. Since clubs, parties, and raves also tend to feature freely flowing alcohol, it is not unusual for attendees to mix their party drugs with booze. This combination is responsible for thousands of ER visits every year and more than a few overdose deaths.

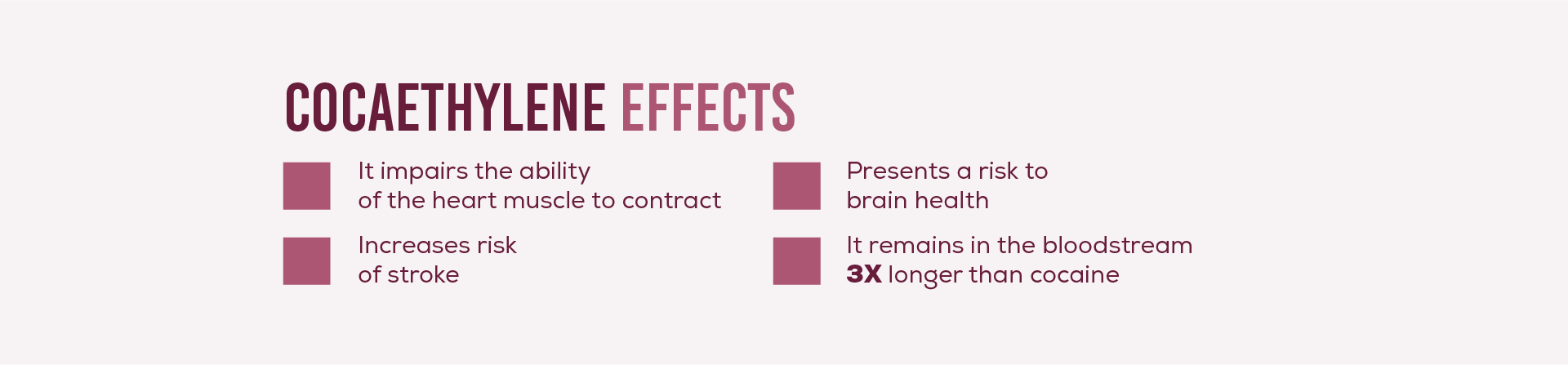
The combination of cocaine and alcohol in particular creates a unique risk due to an interaction within the liver. When the liver metabolizes alcohol and cocaine at the same time, a chemical called cocaethylene is produced as a byproduct. When cocaethylene is leached into the bloodstream, it can do irreparable damage to the heart over time and also presents a risk to brain health. Cocaethylene remains in the bloodstream three times longer than cocaine.
When an intense stimulant is mixed with a CNS depressant, the resulting contradictory influences put a great strain on the heart. Cardiac arrest is often the result of a stimulant and alcohol overdose. Other side effects may include:
Meth is also a stimulant, like cocaine, but its chemical composition and effects are somewhat different. Meth users usually treat depressants differently than do cocaine users. Alcohol sometimes becomes part of the meth binge cycle during which a user will stay awake for days, "tweaking" on meth. Eventually they have to sleep, so they use alcohol or another CNS depressant to force their body into a substance-induced sleep after a binge. This is an incredibly unhealthy and perilous cycle.

Besides the risk of cardiac arrest that comes from mixing alcohol with stimulants, this situation leads to the added risk of alcohol poisoning. Meth use can hide the symptoms of drunkenness, so if you mix the two, you may not notice that you're becoming drunk. You continue to drink more and more, searching for the sleepy euphoria that alcohol brings, only to overdose on the alcohol before you notice its effects. This mix can bring about other consequences as well:
Hallucinogens, or psychedelic drugs, include a variety of substances that bring on hallucinations, visions, and out-of-body experiences. Some of these include:
These substances vary greatly in their chemical compositions, and so each one has a different interaction with alcohol. There is very little existing research on the effects of mixing hallucinogens with alcohol, but most experts agree; don't do it. The most common side effect is a "bad trip" or extremely unpleasant delusions. Other possible results of mixing these substances are:
Whether it happens by accident or intentionally, mixing alcohol with other substances is a high risk behavior that could easily result in overdose. If you or someone you know is in the habit of abusing multiple substances on a regular basis, the risk is much higher. Become acquainted with the signs of overdose and how to react if the worst happens.

First, know what an overdose looks like. These are some telltale signs:
If the day comes when you notice someone exhibiting any combination of these symptoms, don't hesitate. Call an ambulance or, if possible, rush the overdose victim to the closest emergency room right away. If you have to wait for emergency medical help to arrive, there are a few things you can do in the meantime:

If someone you care about has a polydrug addiction, time is of the essence. Any addiction that involves mixing various substances - be it alcohol, prescriptions, or illicit drugs - on a regular basis is a dangerous addiction with high chances of overdose.
Keep in mind; polysubstance abuse can lead to an addiction that is even stronger and more severe than a single-substance addiction, and the addict may be intensely resistant to drug treatment. If this is the case, the only way to help may be to organize an intervention - an initiative that will require some well-planned preparations in order to work:
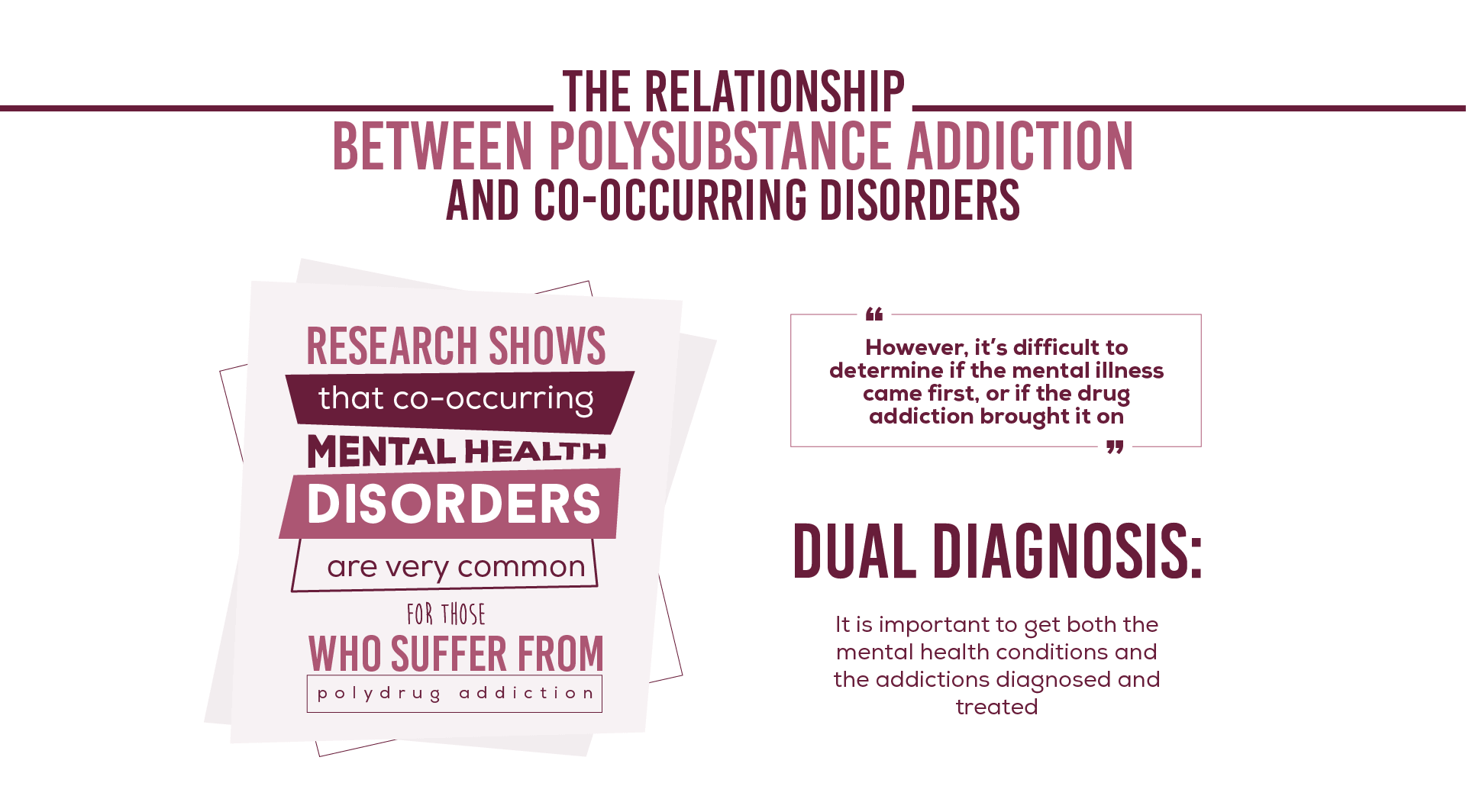
Polysubstance addiction can occur when any two substances are mixed and consumed on a regular basis. Any kind of polysubstance abuse is dangerous, and if it involves alcohol with other substances, it may be even more unpredictable. Research shows that co-occurring mental health disorders are alarmingly common for those who suffer from polydrug addiction, but it is difficult to determine if the mental illness came first, or if the drug addiction brought it on.
In cases of patients who take medication on a daily basis for social anxiety and then develop a problem with alcohol abuse, it is clear that the anxiety condition came first.
On the other hand, someone who abuses ecstasy and alcohol on a regular basis may actually develop mental depression as a result of how the two substances affect the brain's serotonin levels.
Irregardless of which problem came first, the important thing is to get both the mental health conditions and the addictions diagnosed and treated. At a high-quality drug rehab facility, you will be given a variety of health, biosocial, and psychiatric examinations to diagnose any co-occurring mental or emotional conditions that underlie your addiction.

After a dual-diagnosis has been made, a team of doctors, addiction specialists, and counselors can formulate a personalized treatment plan that addresses both the addiction and any co-occurring mental health disorders at the same time. Dual-diagnosis treatment has been shown to be a great deal more effective than treating either addiction or mental illness on its own.
No matter what kind of addiction is involved, withdrawal is a painful and unpleasant experience. Alcohol withdrawal in particular is notorious for its sheer difficulty. Once additional substance addictions are added on to the process, it becomes exponentially worse.
Every substance comes with its own withdrawal symptoms. The symptoms of alcohol withdrawal are mostly physical in nature, while stimulants like cocaine cause emotional withdrawal symptoms. If you have to go through withdrawal from both substances at the same time, you would be bombarded by all of the withdrawal symptoms from both the alcohol and cocaine addictions, creating a new and unique level of suffering.
What's more, detoxing from multiple substances at once can actually be dangerous. Certain types of polydrug abuse do great damage to the brain, kidneys, liver, and heart. When this is the case, doctors must be especially careful how they treat the withdrawal symptoms, since certain detox medications cannot be administered to a patients in poor physical health. Certain treatments or medications could actually cause additional damage or side effects if not properly regulated.
For polysubstance detox, it is especially important to undergo a withdrawal process under the supervision of doctors who are familiar with your health status and types of addiction. In this way, the right team of specialists can formulate a detox plan that will be as safe and comfortable as possible.
Especially for addictions that involve multiple substances, medical detox could be a viable option to make polydrug withdrawal more bearable. Through a careful combination of medication and therapeutic activities, a professional drug detox facility can help to soothe withdrawal symptoms and reduce the chances of relapse. When alcohol addiction is an issue, certain medical prescriptions can also prevent dangerous withdrawal conditions like delirium tremens.
Polysubstance withdrawal can be complicated, however, because of its effects on the brain and organ systems in the body. Medically assisted detox should only be performed with the help of experienced medical professionals to ensure your safety and prevent dangerous drug interactions or side effects.

Completing detox is a huge step in the recovery journey, but it is by no means the last one. Only 15% of people who complete detox alone achieve long-lasting sobriety, as opposed to 46% for people who complete drug rehabilitation treatment.
This is because detox only eliminates the physical side of addiction, but there are psychological factors that attribute to addiction as well; and these cannot be ignored. Once your body has shed its physical dependence to multiple substances, there will be more hard work to do in order to prepare your mind and lifestyle for a lifetime of recovery.
Drug rehab will help you to identify the causes and nature of your addiction. From there, you can analyze your triggers and cravings, exploring the best ways to cope with your own personal addiction and the challenges that lay ahead. Not only does a good drug treatment program give you great insight into your own strengths and weaknesses, it also provides you with a range of tools that will help you to stay sober through the days, months, and years of recovery that await you.
Judy Garland once said, "I'm not telling you it's going to be easy; I'm telling it's going to be worth it." These words are especially poignant when applied to addiction recovery. It won't be easy, especially in the case of polydrug abuse, but a lifetime free of addiction will always be worth the struggle. You are worth it.

Our admissions coordinators are here to help you get started with treatment the right way. They'll verify your health insurance, help set up travel arrangements, and make sure your transition into treatment is smooth and hassle-free.
[DirectNumber] Contact Us