“It is clear that individuals who use multiple substances are at elevated risk of developing comorbid psychiatric and other health conditions. They also have more pervasive deficits in cognitive functioning that place them at elevated risk of poorer treatment outcomes.” ~ J. Connor, M. Gullo, A. White, and A. Kelly, Polysubstance Use: Diagnostic Challenges, Patterns of Use, and Health It is hard enough to recover from an addictive disorder when there is only one substance involved. When one, two, three, or even more substances are involved, the difficulties are magnified, as are the dangers.
What Is Polydrug Abuse?
 The best definition of polydrug abuse is the concurrent use of more than one intoxicating substance, with actual physical dependence on at least one. Sometimes, one substance is the preferred “drug of choice”, and the other substances are used to enhance its effects, but other times, there is no single “preferred” drug, and the substance abuser is prone to using whatever substance is available. It is important to note addiction is never about the drug of choice. Rather, addiction is a disease that is caused by a profound, unattainable craving resulting from a combination of factors that are unique to the individual:
The best definition of polydrug abuse is the concurrent use of more than one intoxicating substance, with actual physical dependence on at least one. Sometimes, one substance is the preferred “drug of choice”, and the other substances are used to enhance its effects, but other times, there is no single “preferred” drug, and the substance abuser is prone to using whatever substance is available. It is important to note addiction is never about the drug of choice. Rather, addiction is a disease that is caused by a profound, unattainable craving resulting from a combination of factors that are unique to the individual:
- Physical – Drug use causes changes within the user’s brain. As a result, the person is physically compelled to seek and use intoxicating substances again and again, regardless of negative consequences to the rest of their life.
- Mental – Addiction often co-occurs with other mental/psychiatric disorders, such as anxiety, depression, PTSD, or bipolar disorder. Sufferers of these conditions will often “self-medicate” in an effort to feel better.
- Emotional – Many people who abuse alcohol or drugs do so as a means of coping with some past traumatic event – childhood neglect or abuse, sexual or violent assault, or combat, for example.
How Big of a Problem Is Polydrug Abuse?
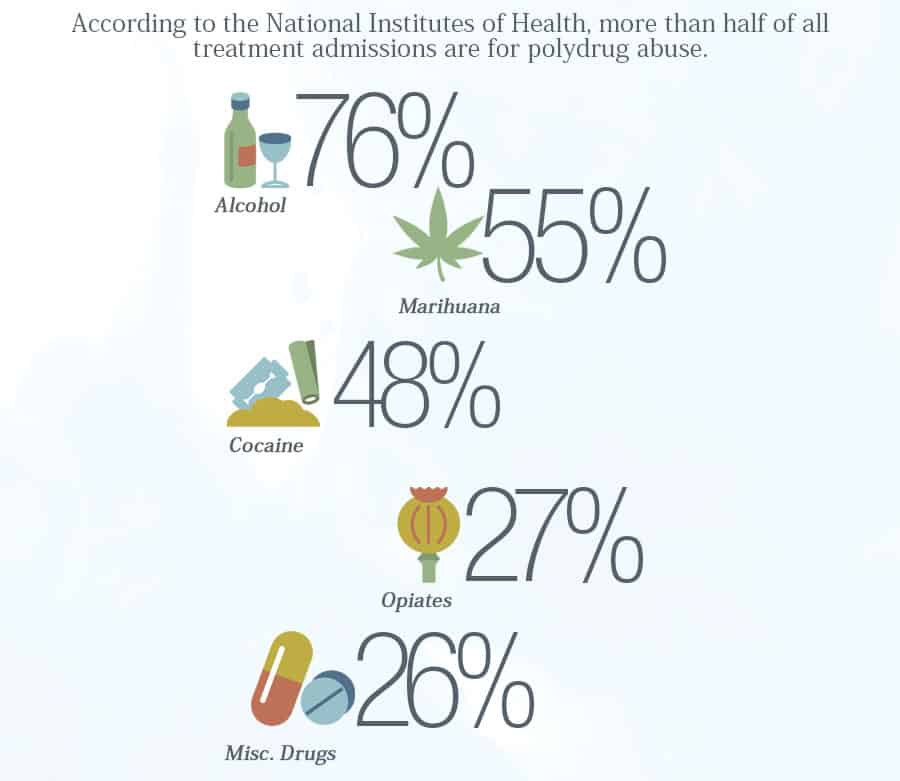 According to the National Institutes of Health, more than half of all treatment admissions are for polydrug abuse. Among the 56% of treatment admissions who self-reported polydrug abuse:
According to the National Institutes of Health, more than half of all treatment admissions are for polydrug abuse. Among the 56% of treatment admissions who self-reported polydrug abuse:
- 76% abused alcohol
- 55% abused marijuana
- 48% abused cocaine
- 27% abused opiates
- 26% abused other drugs
The Role of Alcohol in Polydrug Abuse
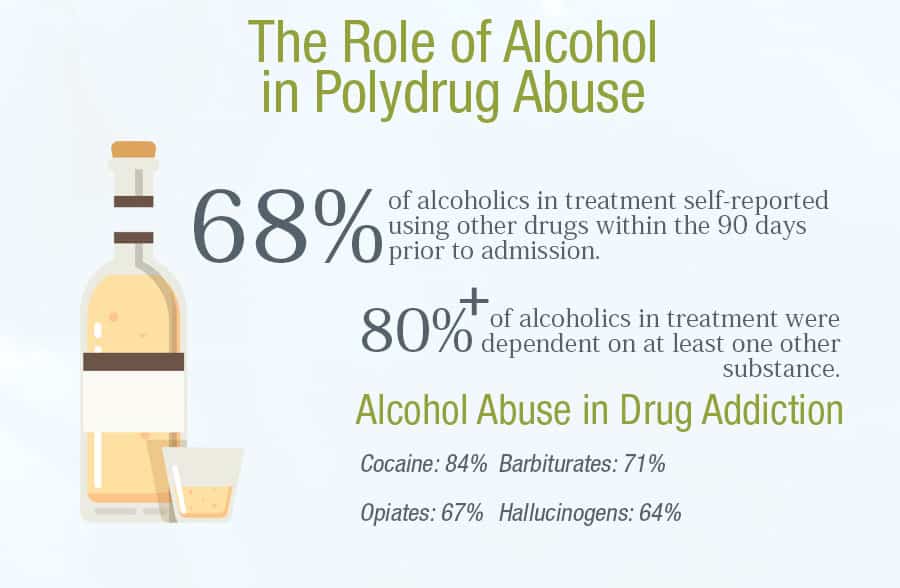 Alcohol seems to be substance most-frequently associated with polydrug abuse:
Alcohol seems to be substance most-frequently associated with polydrug abuse:
- 68% of alcoholics in treatment self-reported using other drugs within the 90 days prior to admission
- Over 80% of alcoholics in treatment were dependent on at least one other substance
- Among individuals in treatment for an illicit drug, alcohol abuse is extremely common:
- Cocaine – 84%
- Barbiturates – 71%
- Opiates – 67%
- Hallucinogens – 64%
The Role of Benzodiazepines in Polydrug Abuse
Benzodiazepines are also an increasingly popular choice for polydrug abusers. Per a recent study published in the American Journal of Public Health, benzodiazepines–tranquilizing medications such as Xanax and Valium –were a factor in 31% of the nearly 23,000 drug fatal overdoses in America in 2013. Combining “benzos” with other substances prolongs the euphoric high. Over the last 20 years, one of the most popular polydrug combinations has included benzodiazepine and opioids. The Substance Abuse and Mental Health Services Administration reported that in 2011, benzodiazepine/opioid combinations made up the majority of ER visits due to the nonmedical use of psychotherapeutic medications.
- Heroin abusers self-report “stronger and longer” effects when combining heroin and flurazepam intravenously.
- Three-quarters of heroin users report benzodiazepines during the previous year.
- 25% of heroin users reported using benzos daily.
- A third of heroin users had a legitimate benzodiazepine prescription within the previous 30 days.
- Approximately 40% of patients in opioid maintenance programs had a valid benzodiazepine prescription within the previous 12 months – a rate that is 8X that of the general population.
- 50% of new admissions to methadone clinics need to benzodiazepine detoxification.
- As much as 70% of patients in methadone programs test positive for benzos.
- Almost 75% of patients in methadone programs who are concurrent benzo users report that diazepam magnifies the effects of their daily methadone dose.
- 94% of methadone patients will also use sedatives during their lifetime.
- Up to 60% of chronic pain patients will use benzos on a regular basis.
- Approximately 16% of patients on opioid pain medications test positive for benzodiazepines.
Why Is Polydrug Abuse So Dangerous?
The abuse of multiple substances can be extremely hazardous, for a number of reasons:
- In combination, different substances can magnify each other’s effects – too dangerous, even deadly levels. Example – alcohol, opioids, and benzodiazepines.
- In contrast, some substances will mask the effects of other drugs used concurrently, so the person takes more and more – to the point of overdose. Example – stimulants and opioids.
- A person may experience cognitive/memory impairment while under the influence of one substance and “forget” how much of the other substance they have taken. Example – alcohol and prescription medications.
The use of multiple drugs is a factor in almost 75% of all drug overdoses, and in up to 98% of overdoses that prove fatal.
What Is the Best Strategy for Recovering from Polydrug Abuse?
 All addictive disorders affect the reward areas of the brain. This means that the ability to choose whether or not to use and intoxicating substance – when or how much – is no longer under the control of the individual. When a person is in the grips of active addiction, their best chance of a successful recovery is with professional help from trained addiction specialists in a properly-accredited drug/alcohol rehab facility. Through a combination of medication, individual counseling, peer group therapy, behavioral modification, and ongoing support, the disease of addiction is addressed on multiple levels until a person can better manage their condition.
All addictive disorders affect the reward areas of the brain. This means that the ability to choose whether or not to use and intoxicating substance – when or how much – is no longer under the control of the individual. When a person is in the grips of active addiction, their best chance of a successful recovery is with professional help from trained addiction specialists in a properly-accredited drug/alcohol rehab facility. Through a combination of medication, individual counseling, peer group therapy, behavioral modification, and ongoing support, the disease of addiction is addressed on multiple levels until a person can better manage their condition.

