Another year is upon us. If you are in recovery from substance addiction, you may have resolved to focus harder, try harder, on your sobriety and well-being, as the previous year was marred by unresolved triggers and, quite possibly, the inevitable relapse, along with the heady mix of emotions associated with both of these things that you may have had to deal with too. As any person in the process knows, the risk of relapse, which every recovering addict needs to know like the back of their hand, is at its most likely when an addict:
- Lacks support (or chooses to forego the support out there),
- Has zero accountability to anyone else, and
- Refuses an ongoing relationship with the recovery process in general; for example, not following the guidelines provided by their respective addiction treatment professionals, even their own physicians, choosing not to attend support groups, such as AA or NA, and so on.
Some recovering addicts even decide that now, as they are sober and not drinking or using, they are, in some way, cured. Those in recovery who feel they can now turn their backs on a continued effort to stay clean and sober are setting themselves up for potential and damaging relapse. In some cases, this has proven to be fatal. The beginning of a new year usually brings a sense of purpose to a person. However, those who have nailed their flags to the mast, and announced a resolution to do whatever, are 90% likely to not last even this month, and another New Year’s resolution hits the dirt. For the recovering addict, and as highlighted already in this introduction, a lack of purpose when it comes to recovery from addiction never ends well. Furthermore, the most ardent of those in recovery, armed with dedication, resolve and coping mechanisms in abundance can still be susceptible to relapse.

Why Do Recovering Addicts Relapse?
According to the National Institute on Drug Abuse (NIDA), between 40-60% of recovering addicts will experience a relapse. If that sounds a little high to you, even a little deflating, think of it this way – substance addiction’s recurrence rate of around half is similar to those of other chronic diseases, including hypertension and Type I diabetes. So what exactly causes around half of those in recovery to relapse back into an addictive behavior they are trying desperately to avoid? Because there are so many initiating factors to the disease in the first place, such as genetics, family history, environment, and so on, a relapse, when viewed in hindsight by addiction specialists, will unlikely lead to a 100%-accurate cause for occurring. Throw in the fact that we all have differing circumstances, and you see how difficult it becomes. However, when this is actually attempted, the primary attributable reason is usually a simple one – stress, or, more exactly, a recovering addict’s inability to deal effectively with stress, and to the point of relapsing into the past addictive behavior, they are trying to avoid. Obviously, if you add a lack of a healthy support system into this loose equation, the chances of a relapse occurring are increased significantly. One additional factor not considered as yet is the one of familiarity. Because an addict’s previous substance use is associated with particular and definite outcomes, there can be the inherent need to return to that which is familiar in times of stress. These outcomes include:
- Feelings of euphoria
- Increased confidence (or its perception)
- Feelings of belonging (related to other users)
- The attraction of the addiction
- Personal physiological feelings, and
- The ability to rely upon these outcomes
Relapse is a Setback – It is Not Failure
Does the hypertensive patient who experiences an unexplained surge of sky-high blood pressure, and even chest pains, think to themselves, “This treatment isn’t working for me – time to forget treatment, eat, drink and exercise how I like, even if that equates to an early death”? Or does the Type I diabetic just think, “Forget the insulin, bring on the chocolate ice-cream and let my blood glucose levels run free!,” if they experience an unexplained setback of some description? A little extreme, perhaps, but it is actually an identical point. Substance addiction cannot be cured, just like the hypertension and the diabetes above; however, it can be successfully controlled through continuous treatment and complete abstinence from the substance concerned. Medically and simply defined, addiction is “a chronic, relapsing brain disorder.” Often, at its very root, a psychological catalyst exists that initially drives them towards the addiction. This catalyst, such as trauma or grief, and so on, becomes a powerful influence over their addiction, and possibly other areas of their lives, and can finally manifest itself into mental health disorders, such as obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), and other mood and behavior disorders. The existence of a medically-diagnosed mental health disorder along with a substance addiction is known as a co-occurring disorder (also known as dual diagnosis). Unless this other disorder has been treated simultaneously along with the addiction, it will become an extremely powerful trigger to relapse, and a constant one at that. The complexity of a mental disorder often drives an individual to self-medicate, and then to participate in high-risk behaviors, both of which are potent triggers in themselves.

What is a Relapse Trigger?
Relapse triggers are varied, personal and, clearly, potentially dangerous to those in recovery. They can be either internal or external in nature, and will center around one of the following:
- Thoughts
- Feelings
- Sensations
- Situations
- Relationships, or
- A combination of more than one of these
Furthermore, they can also be strongly influenced by the presence of other mitigating factors, such as feeling stressed, tired, or unwell, either physically or mentally. Nobody expects any addict to be aware of every possible trigger, but they should be aware of every possible trigger that is personal, relevant and potentially dangerous to them. Learning how to effectively cope and deal with the relapse triggers that are pertinent to them will enable recovering addicts to be at least prepared for them.
What are Internal Triggers?
Internal triggers are the emotions that are evoked by thoughts of previous substance abuse, and a recovering addict’s exposure to these cues may cause them to first crave, and then use substances. Emotions that can act as internal triggers include: 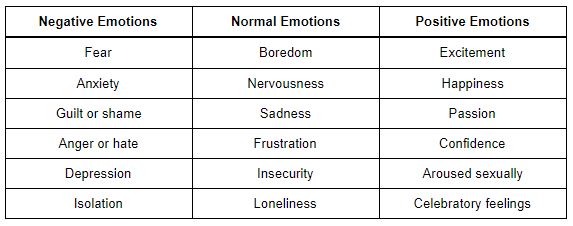
What are External Triggers?
External triggers are people, places, situations (including certain activities), and even objects that, like emotions, evoke thoughts of previous substance abuse, and again may cause cravings, and subsequent substance abuse. When an addict is in an addiction rehab facility, these external triggers are removed, and so allow the individual to work on coping skills to deal with such triggers, for when they leave treatment. Furthermore, certain external triggers can provoke a subconscious response, meaning that the recovering addict is reinforcing a desire to resume substance abuse without them even realising that’s happening. A NIDA study on one external trigger – cocaine-related imagery – found that the emotional centers of ex-addicts’ brains were stimulated when these individuals looked at the images, setting off a rapid activation of the circuits associated with substance cravings. The study concluded that it was beneficial for recovering addicts to completely avoid the people, places, situations, and objects, ie. the external triggers, that reminded them of their past substance abuse. Examples of external triggers can include:
- People: Sadly, those closest to us can be the most likely people to instigate a relapse, especially if they are drinking or using. Even a complete stranger can be a trigger if they are offering “just one drink” or “just one puff.” Primary examples include former dealers, family, friends, spouses/partners, and familiar neighbors.
- Places: Places where you have previously drunk or used a highly perilous to your sobriety – even just driving through an old haunt can form a trigger related to past substance use. Examples of places to steer clear of include bars, clubs, parks, concert venues, friends’ houses.
- Situations: Social settings or particular events, such as parties, family celebrations, weddings, payday, New Year’s Eve, and holidays.
- Objects: Sometimes, the simplest object, even as just a piece of garbage, can be a cue to previous substance use, such as drug paraphernalia, spoons, ATMs, credit cards, and empty prescription bottles/packaging.
IMPORTANT: It is advisable to remember that the triggers alone rarely initiate immediate use. Normally, when those in recovery succumb to their personal triggers, a period of time elapse where the individual`s brain attempts to create reasons, even logical-sounding ones, to use substances again, despite their clear intention not to do so. That is the power of addiction over you. This unseen and ongoing mental battle will obviously increase their vulnerability to substance cravings, and will sometimes result in the clear potential for relapse.

The 3 Stages of Relapse
Substance addiction relapse occurs in 3 distinct stages or phases – the emotional stage, then the mental stage, and finally, the physical stage. Contrary to what you may think or have heard, relapse is far from quick – it is a slow process, where the individual goes through each stage, as opposed to a rapid event. For the recovering addict, simply being aware of these 3 phases of relapse can help prevent one before it actually occurs.
First Stage: Emotional Relapse
A potential relapse begins when the individual is not actively thinking about or considering using drugs or alcohol at all. However, their emotions, and subsequent behaviors, may be setting the wheels of relapse in motion. Warning signs of this first stage include (but aren’t limited to):
- Bottling up emotions
- Missing recovery support group meetings
- Subconsciously Isolating yourself from family and friends
- Poor nutrition and sleep
- Lack of hygiene
- An inability to manage strong emotions, such as stress, anxiety, and anger
Using a daily journal to keep track of yourself is an excellent way to self-reflect, and is an essential tool during recovery. The journal will help you to understand if you are in the emotional stage of relapse. Be truly honest with how you feel, as denial is an important element of this stage.
TED Talk: “Relapse Is Part of Recovery” – Hufsa Ahmad
Second Stage : Mental Relapse
If we ignore the signs of an emotional stage (or simply decide to not address them effectively), there is an increased risk of transitioning to the second stage of relapse – mental relapse. Once you are in this stage, unless you act, you are at a high risk of substance addiction relapse. This stage is best described as a tough mental struggle with yourself – the addicted side of you yearns to fulfil your cravings, and the sober side wants nothing to do with them. Please remember that occasional thoughts of using substances are quite normal in early recovery; however, these aren’t those type of thoughts – they feel more like a serious consideration. Signs of this mental relapse include:
- Cravings to use substances again
- Consciously thinking about people, places, and things associated with past use (your external triggers, if you like)
- Socializing with substance-using people from your past
- Minimizing or glamorizing or fantasizing about your past use
- Lying and/or scheming
- Actually planning your relapse
It is essential that you speak with an addiction specialist, your sponsor or a trusted other, as this stage is absolutely critical to your continued sobriety. Additionally, remember that cravings only last approximately 15-30 minutes, and you can use relaxation techniques, such as mindfulness or yoga, to calm yourself and get refocused on your recovery.
Third (& Final) Stage: Physical Relapse
If a recovering addict reaches this point, a relapse back into substance use is not a foregone conclusion if they seek the help and support that they need – now. However, a failure to do this, or let alone acknowledge an issue still doesn’t exist, will usually end in the unwanted relapse, as this stage normally occurs quite rapidly. It is very nearly too late unless you take immediate action.

8 Dangerous Triggers You Must Avoid in 2020
For the vast majority of people, the beginning of a new year is a new and fresh start, and a time of hope. For the recovering addict, it may well signal the same, but, as they are already sober, it is best to look upon it as a firming up of new or continued positive behaviors, new or continued healthy routines, new or continued relaxing activities, and new or continued ways of ensuring you are looking after both your mental and physical health. New Year’s Eve has now come and gone (safely, it’s hoped), and the year is spread out before you. However, as any successful recovering addict will happily tell you, now is definitely not the time to feel complacent in any way or begin to feel like you’re halfway there. Addiction has no cure, you’ll never get an “all clear” from your family physician, and so all you can do is stick to whatever program you believe and trust in – whether it’s the 12 steps, another guided program, or your own, self-managed way of keeping clean and sober. As the saying goes, “Whatever works…” Because, quite simply, work it surely must. What follows is our list of “8 Dangerous Triggers to Avoid in 2020.” It’s not definitive, and it’s certainly not personal to you – only you know exactly what relapse triggers exist for you. However, it is our guide about the common potential dangers to sobriety that exist at the beginning of a new year.
8 Dangerous Relapse Triggers in 2020
#1. Negative Emotions: Recovering addicts who are early on in the process (or newly-sober past substance users) will have a whole host of negative emotions circulating around their mind. Yes, they may well feel motivated and hopeful, but they are just as likely to be experiencing some level of sadness, anger, guilt, shame, and loneliness. It is imperative that these emotions are seen as normal, so the newly sober former addict must work on coping with these strong feelings. #2. Stress: Often at the root of many relapses, stress should always be seen as a potential danger to recovery. In fact, it could well be the No. 1 trigger because of its broad range of effects on the mentally and physically. Feeling financial strain, increased responsibility at work or home, and health problems left over from the substance abuse can all lead to stress. The newly sober and those early in recovery need to ensure they manage the stress in their lives effectively. #3. Overconfidence: A new year can bring a brighter outlook. However, becoming overconfident, because of this brighter outlook (seemingly to everything), in your recovery particularly puts you at risk of relapse. Having self-confidence is welcome, but overconfidence, especially to the point of complacency, is simply dangerous. Never think to yourself that you are “cured” – you can never be cured of addiction. To stay in the good place you currently are, you need to remain in your recovery program, and doing all the things that keep you healthy. With complacency, there is the risk you will expose yourself to high-risk situations – and that really is dangerous. #4. Physical Illness / Mental Disorder: Physical illness, especially if it involves a noticeable level of pain, will unduly stress your body. By advising your physician that you are in recovery from substance addiction If they don’t already know), and then being insistent about being given non-addictive prescriptions, you are safeguarding your recovery from unnecessary risk. Likewise, a mental disorder, either relatively new or an undiagnosed existing one, will stress you mentally, as well as you having to deal with the nature of the disorder, eg. depression, anxiety, or a mood disorder. Seek treatment immediately if this is the case. #5. Social Isolation: It cannot be stressed more strongly how important a strong and reactive support system is for those in recovery, regardless of whatever stage of recovery that is. Failure to ensure that’s the case, or simply being reluctant to reach out, will make you feel isolated. Anxiety over social situations can be worrisome for newly sober addicts, and so you should consider a support network one of your main priorities. #6. Sex / Intimate Relationships: Yes, the very same. Often ignored at the beginning of recovery, the advice is clear – try to avoid intimate or sexual relationships during your first year. In fact, some say, “Relationships = Relapse.” The breakdown of a new relationship will affect you emotionally much harder than normal. Additionally, some recovering addicts use a relationship as their new addiction. Be careful. #7. Increased Responsibility: It may seem paradoxical, but positive life events can also be relapse triggers. How you celebrate such an event can also be risky. Increased responsibility, especially in the workplace, normally brings additional pressure and stress. Only accept new responsibility if neither of these will apply. #8. Thinking About or Glamorizing Past Substance Use: Relapse is a slow, long process. At times, you will think about your past substance use. It is vital to put these thoughts in the proper perspective. Remember, as mentioned previously, such thinking can lead to your brain subconsciously planning a relapse. If you find you are doing this, speak up! Talk to a counselor, sponsor or close friend. Remember, you chose a life in recovery because there was nothing else. If you are concerned that you or a loved one is close to an inevitable relapse back into substance use, please do not delay. Contact your support network immediately and follow their guidance, or call a member of our experienced team here at Northpoint Washington – it could be one of the most important things you ever do.

